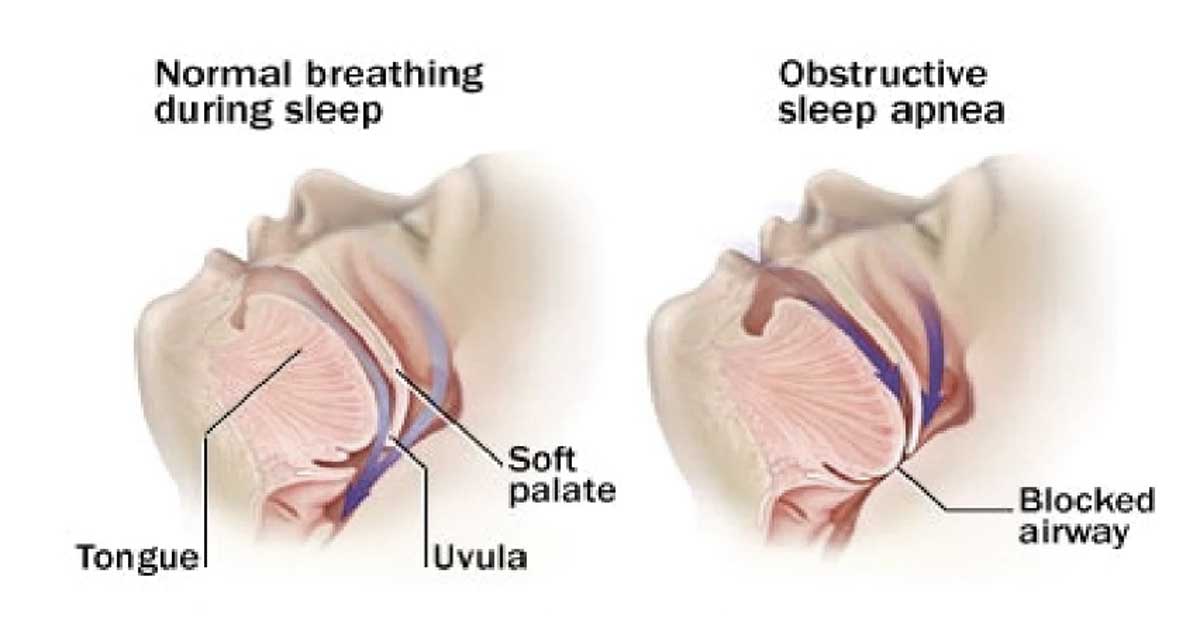
The causes of apnea can vary depending on the specific type of apnea being referred to. The two primary types are obstructive sleep apnea (OSA) and central sleep apnea (CSA). Here are some of the common causes associated with each:
Obstructive Sleep Apnea (OSA):
Central Sleep Apnea (CSA):
It’s important to note that these are general causes, and individual cases of apnea may have additional contributing factors. If someone suspects they have sleep apnea, it is recommended to consult a healthcare professional for a proper evaluation and diagnosis.
The symptoms of apnea, particularly obstructive sleep apnea (OSA), can vary among individuals. Some common signs and symptoms associated with apnea include:
It is important to note that not everyone with apnea will experience all of these symptoms, and the severity can vary. If you or someone you know is experiencing these symptoms and suspect apnea, it is advisable to seek a medical evaluation from a healthcare professional, such as a sleep specialist, for proper diagnosis and treatment.


It is essential to address and treat apnea to restore normal breathing patterns, maintain adequate oxygen levels, and minimize the associated health risks. Treatment options such as continuous positive airway pressure (CPAP) therapy or other interventions can help improve oxygenation, alleviate symptoms, and reduce the long-term impact of apnea on the body.
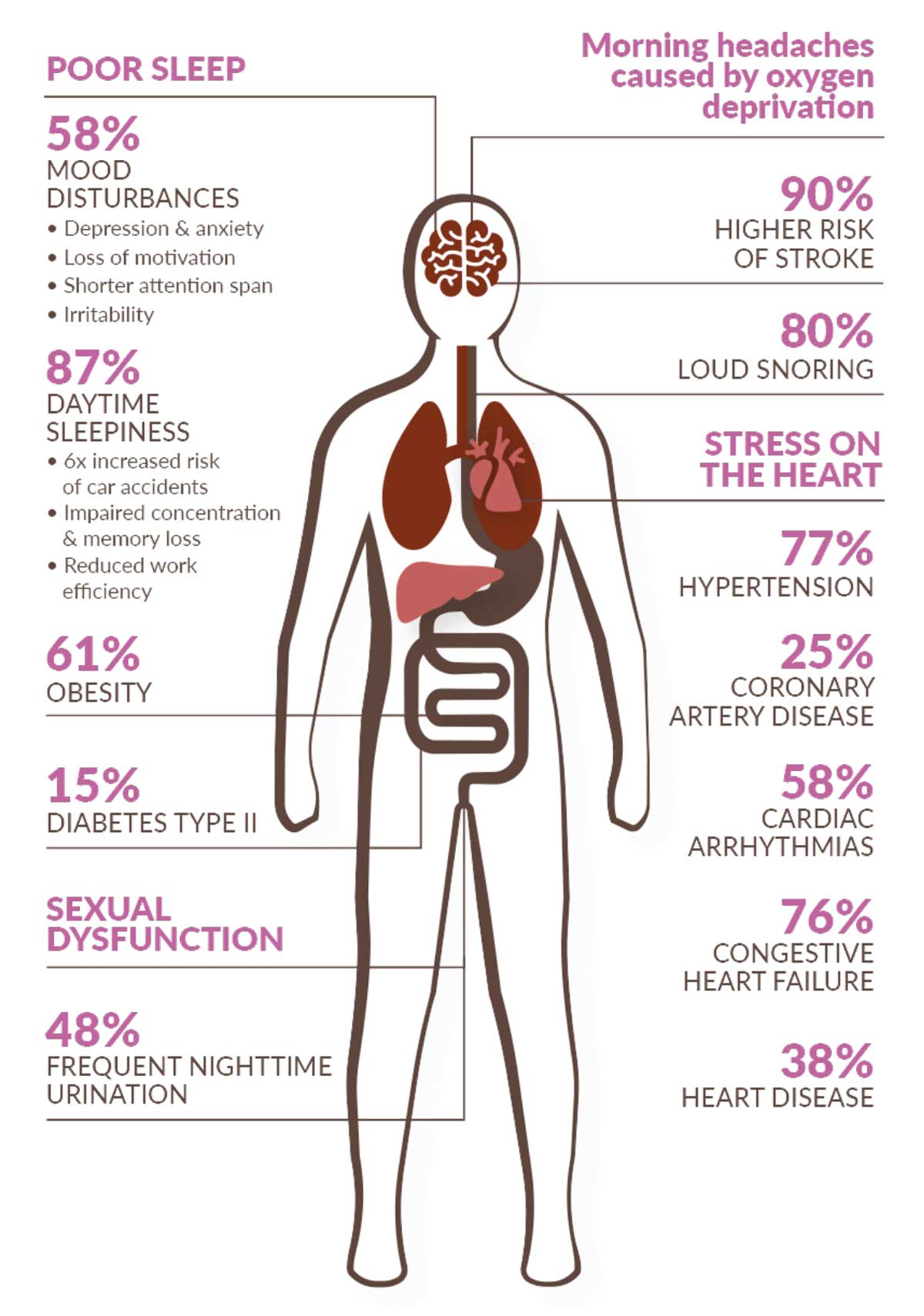
Yes, apnea, particularly obstructive sleep apnea (OSA), can be dangerous if left untreated. It can have a significant impact on a person’s overall health and well-being. Here are some potential risks and complications associated with untreated apnea:
It is crucial to recognize the potential dangers of untreated apnea and seek medical evaluation and treatment. With appropriate management, including lifestyle changes, use of continuous positive airway pressure (CPAP) therapy, or other interventions, the risks and complications associated with apnea can be significantly reduced, improving overall health and quality of life.
Several machines and devices are commonly used in the diagnosis and treatment of apnea, particularly obstructive sleep apnea (OSA). Here are some of the necessary machines and devices:
The specific machines and devices required depend on the purpose, whether it is diagnosis, monitoring, or treatment. It is important to consult with a healthcare professional, such as a sleep specialist or pulmonologist, who can determine the appropriate equipment based on an individual’s specific needs and circumstances.
Copyright © 2023 Apneas. All rights reserved.
No products in the cart.